Research team tests novel immunotherapy against certain blood cancer cells

Acute lymphoblastic leukemia (ALL) is the most common cancer in children. This form of blood cancer is caused by malignant abnormal precursor cells of certain white blood cells, and usually leads to a rapidly progressive reduction of bone marrow function, and thus impaired blood formation. If left untreated, it quickly leads to death. Despite the severity of the disease, in many cases children today have good chances of survival and being cured. The current standard treatment consists of various forms of chemotherapy, but these cause severe side-effects because of their toxic effect on healthy cells, too.
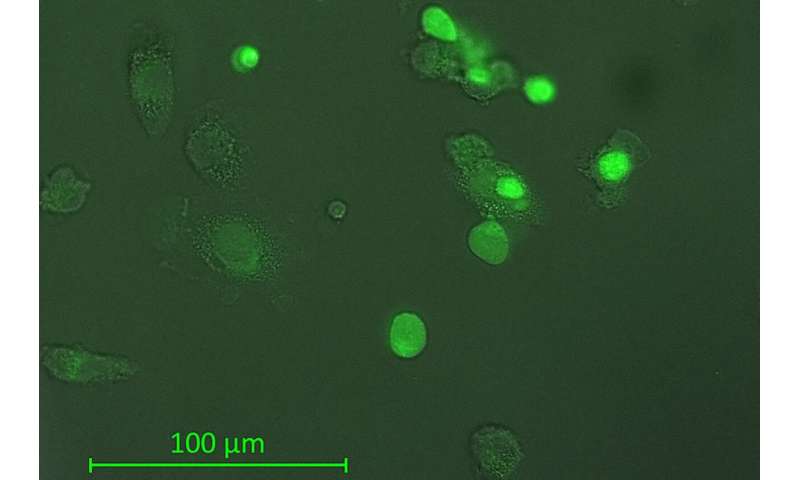
In addition, a certain proportion of the young patients—about 15 to 20 percent—do not respond to treatment in a sustained manner. Scientists from the Faculty of Medicine at Kiel University (CAU) and the Department of Pediatric and Adolescent Medicine I at the University Medical Center Schleswig-Holstein (UKSH) Campus Kiel are therefore exploring alternative forms of treatment, in particular different variants of immunotherapy. In a recent preclinical study, they examined the antibody daratumumab, which has already proven successful against another type of cancer. They hoped for a possible suitability to combat blood cancer cells in a subtype of ALL, the so-called T-cell ALL (T-ALL). To date, there is no form of immunotherapy for this type of the disease. In model experiments, a complete removal of the cancer cells was achieved in around 50 percent of the cases. Together with their partner research institutions nationwide, the Kiel scientists recently published their latest research results in the renowned scientific journal Blood.
Preclinical model experiments show promising results
In the exploration of new forms of treatment against cancer, immunotherapy with antibodies is among those which show promising potential. This treatment uses artificially produced antibodies, i.e. specific synthetic proteins which work according to the lock-and-key principle. Under certain circumstances, they can help cells of the immune system to recognise and destroy cancer cells. However, in many cases the exploration of the associated treatment options is still in an early stage. PD Dr. Denis Schewe, senior physician for hematology, oncology and stem cell transplantation at the Department of Pediatric and Adolescent Medicine at the UKSH, and his research team carried out fundamental combination experiments on mice using the antibody daratumumab to test for possible effectiveness against T-ALL cancer cells. In doing so, they also compared antibody treatment alone with a combination of antibody and chemotherapy.
“We were able to report initial promising results: half of the animals treated with the antibody showed long term survival, without any signs of disease,” explained the Kiel pediatric oncologist Schewe. It made no difference whether they were treated with the antibody only, or with a combination of chemotherapy and immunotherapy. “The chemotherapy, with its serious side-effects, achieved no improvement, and in the case of our model experiment brought no additional benefits,” said Schewe. However, these experimental results are in no way directly transferable to patients. “Therefore, in the further development of antibody treatment for T-ALL, we must continue to investigate in all directions,” said Schewe.
Translational focus of Kiel’s oncology
The research activities in Kiel’s pediatric oncology are a good example of how fundamental and clinical research cooperate through the Kiel Oncology Network (KON) established at the CAU. For example, KON member Schewe worked closely with Dr. Mildred-Scheel-Haus on a recent study at the USKH. With its Division of Stem Cell Transplantation and Immunotherapy, it also provides treatment for leukemia patients. “Our goal is to further optimize the antibody treatment for T-ALL. In the middle of the year, we were able to raise significant funding from the Deutsche Krebshilfe e.V. (German Cancer Aid) for this purpose,” said Schewe.
Source: Read Full Article




