Readmission risk increases for elderly patients with geriatric-specific characteristics

Researchers have examined new geriatric-specific characteristics that appear to raise the risk of elderly surgical patients having an unplanned hospital readmission within a month of initially leaving the hospital. The new study is published online as an “article in press” on the Journal of the American College of Surgeons website in advance of print publication.
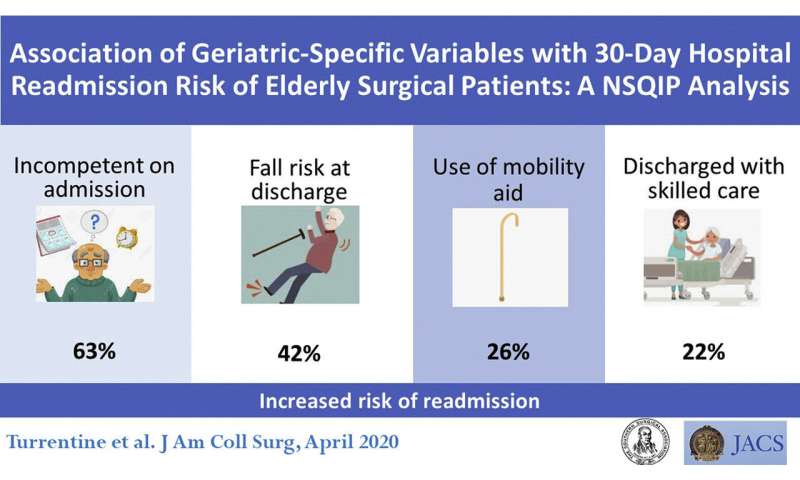
The four geriatric risk factors for readmission after general surgical procedures are cognitive impairment requiring another person to sign the patient’s consent form for the operation (called “incompetent at admission”), use of a mobility aid, risk of falling at discharge from the hospital, and need for skilled home health care after going home.
“Our findings could impact clinical practice,” said Florence E. Turrentine, Ph.D., RN, lead study author and associate professor in the department of surgery at the University of Virginia, Charlottesville. “It is not clear that hospitals are using geriatric variables in evaluating patients. Our results support screening for use of a mobility aid or having a surrogate sign consent when hospitals admit geriatric patients for surgical care.”
Elderly individuals—those age 65 years or older—make up 43 percent of Americans undergoing an inpatient operation* and are more likely than younger patients to have postoperative complications, results of multiple studies show. More than one in 10 of the elderly patients in the new study had an unexpected readmission, according to study authors.
“Readmissions are stressful and expensive and Medicare reduces payments to hospitals with excess readmissions,” said R. Scott Jones, MD, MS, FACS, a study coauthor and emeritus professor and chair of the University of Virginia’s surgery department. “We want to anticipate and hopefully prevent the reasons that contribute to unplanned readmission after an operation.”
The University of Virginia was among 25 participating centers in the Geriatric Surgery Pilot study, which the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) created in 2014 to collect risk factors and outcomes in surgical patients 65 and older. The NSQIP database is the leading nationally validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care in hospitals.
Using the first three years of data from that pilot study, Dr. Turrentine’s research team tested 13 geriatric characteristics and 26 NSQIP risk factors for complications in 6,039 elderly general surgery patients from the NSQIP database.
The investigators evaluated statistically significant predictors of readmission within 30 days following the operation, both overall and for each of five surgical procedure groups. The groups were surgical removal of part or all of the (1) pancreas or liver, (2) colon and/or rectum (comprising 58 percent of the patients), (3) hernia, (4) thyroid or esophagus, and (5) appendix.
Readmission risk factors
Overall, the greatest odds of readmission were with the occurrence of any 30-day postoperative complication (odds ratio 5.1) and the need for a reoperation (odds ratio 2.8)—both NSQIP risk factors. However, the researchers noted their ability to predict readmission risk improved with the added geriatric-specific risk factors. Compared with patients who lacked the risk factor being measured, patients with the following geriatric characteristics had higher readmission odds ratios:
- Incompetent at admission: 1.6
- Fall risk at discharge: 1.4
- Use of a mobility aid: nearly 1.3
- Discharged from the hospital needing skilled care: 1.2
When the researchers looked at geriatric risk factors by procedure type, they discovered that use of a mobility aid had the highest readmission odds for the thyroid/esophagus group (odds ratio 11). The greatest geriatric risk factor they reported for the pancreas/liver group was admission from a place other than home, with a 24.4 odds ratio. In the hernia group, the odds ratio for readmission was 2.2 if they needed a new mobility aid at discharge.
Preventing readmissions
“These study findings give surgeons more information to help elderly patients prepare better for an operation and to find specific ways to prevent unplanned readmissions,” Dr. Turrentine said.
Preparation could include the ACS Strong for Surgery recommendations to improve fitness for an operation, including preoperative rehabilitation, she suggested. For example, she said physical therapy may lessen the chance of needing a mobility aid.
Additionally, some of the identified geriatric risk factors are now part of the NSQIP Surgical Risk Calculator, an online tool providing customized risk estimates for patients planning to have an operation.
Another strategy the researchers proposed to help reduce readmission rates is for the surgeon’s office to check on elderly at-risk patients—especially those who needed a reoperation—by calling them at home after their discharge.
“Our results confirm the need for surgeons to use the geriatric-specific variables to assess the risk for elderly patients undergoing surgical care,” Dr. Jones said. “The ACS is on the right track with its Geriatric Surgery Verification Program.”
Source: Read Full Article




