Cancer DNA blood tests validated by international research team

An international team today reports the findings of an independent assessment of five commercially-available assays for tumor DNA sequencing—a fast, cheap and less invasive method to diagnose and monitor cancer.
The researchers revealed that all assays could reliably detect so-called circulating tumor DNA (ctDNA) when it made up 0.5% of the total DNA in blood, a level of sensitivity that allows detection, genetic analysis and monitoring of late-stage and metastatic tumors.
Published in the journal Nature Biotechnology, the study is a major milestone for the use of ctDNA assays as cancer diagnostics, outlining best-practice guidelines and uncovering key areas of future development.
The research was led by the Garvan Institute of Medical Research, the FDA National Center for Toxicological Research and the University of Arkansas for Medical Sciences. It forms part of the FDA-led Sequencing Quality Control Phase 2 project, which aims to develop standard protocols and quality control metrics for the use of next-generation sequencing in precision medicine, to make it a reality for patients.
“In order for ctDNA assays to be of benefit to patients in the clinic, they need to accurately and consistently detect cancer mutations across different labs and samples. Our study is the most comprehensive evaluation of analytical performance among ctDNA assays to date and represents a significant step forward in the field,” says first author Dr. Ira Deveson from the Garvan Institute.
Next-generation sequencing to monitor cancer DNA
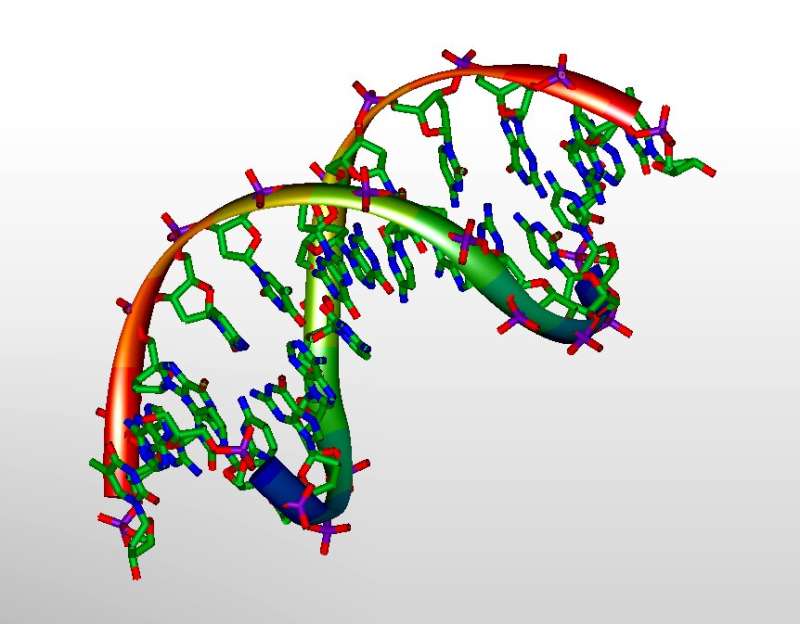
When cancer cells develop, they accumulate mutations in their DNA, fragments of which enter the bloodstream when cancer cells break down. Thanks to assays employing next-generation sequencing, these ctDNA fragments can now be detected in a patient’s blood samples, which could be used to identify and monitor cancer as an alternative to more invasive tissue biopsies.
However, while ctDNA assays are already being adopted in precision oncology clinical trials, researchers and clinicians still lack a thorough understanding of how accurate current assays are, and which aspects of the technology still need to be improved. This knowledge helps define what applications ctDNA sequencing is suitable for and is needed before ctDNA sequencing can be implemented widely in clinical practice.
In their study, researchers from 12 participating laboratories in Europe, Asia and the United States evaluated the performance of current industry-leading ctDNA assays, from companies Roche Sequencing Solutions, Illumina, Integrated DNA Technologies and Burning Rock Dx and Thermo Fisher Scientific.
They tested the assays using synthetic experiments and mock-ctDNA reference samples. Their analysis revealed that all laboratories detected ctDNA mutations above 0.5% relative frequency (consistent with late-stage and metastatic tumors) with high sensitivity, precision and reproducibility using all participating assays. However, the assays detected lower levels of ctDNA (consistent with early-stage cancer or early signs of disease relapse) unreliably and inconsistently between different tests.
In their published paper, the researchers outline priorities for the future development of ctDNA assays, which they say will help advance the technology for clinical applications in monitoring tumor progression, response to therapy and cancer relapse.
“Our findings indicate that the participating ctDNA assays may be suitable for molecular stratification and profiling tumor evolution in advanced cancer patients. This should help clear a path for more advanced clinical trials of ctDNA assays,” says Associate Professor Donald Johann Jr., M.D., from the University of Arkansas for Medical Sciences College of Medicine departments of Biomedical Informatics and Internal Medicine.
“Understanding the current assays’ detection limits was a crucial step towards a future where blood tests can be routinely used as a cancer screening tool. This critical study is a thorough analytical evaluation of ctDNA assays, which defined diagnostic limits, assessed reproducibility and identified key experimental variables that impact performance, and which has been called for by government, regulatory and clinical organizations,” says Dr. Joshua Xu from the U.S. FDA National Center for Toxicological Research.
Source: Read Full Article




