Loss of placental hormone linked to brain and social behavior changes

Preterm birth has been shown to increase the risk of autism spectrum disorders and other developmental problems, particularly in males. The more premature a baby is, the greater the risk of either motor or cognitive deficits. What does the preterm baby lose that is so critical to long-term outcomes?
A new study, in mice, suggests that one factor may be the loss of a placental hormone that the developing brain would normally see in the second half of pregnancy.
The study is the first to provide direct evidence that loss of a placental hormone alters long-term brain development.
In the study, researchers in the laboratory of Anna Penn, MD, Ph.D., now at Columbia University Vagelos College of Physicians and Surgeons and previously at Children’s National Hospital in Washington, D.C., found that reducing amounts of a single hormone, called allopregnanolone (ALLO), in the placenta caused brain and behavior changes in male offspring that resemble changes seen in some people with autism spectrum disorder.
The study also found that both brain structure and behavioral changes in the mice could be prevented with a single injection of ALLO in late pregnancy.
“Our study provides new and intriguing insights into how the loss of placental hormones—which happens in preterm birth or if the placenta stops working well during pregnancy—can lead to long-term structural changes in the brain that increase the risk for autism or other neuropsychiatric disorders,” says lead author Claire-Marie Vacher, Ph.D., assistant professor of neonatal sciences in the Department of Pediatrics at Columbia University’s Vagelos College of Physicians and Surgeons. “What’s encouraging is that these disorders may be preventable if diagnosed and treated early.”
The study was published online August 16 in the journal Nature Neuroscience.
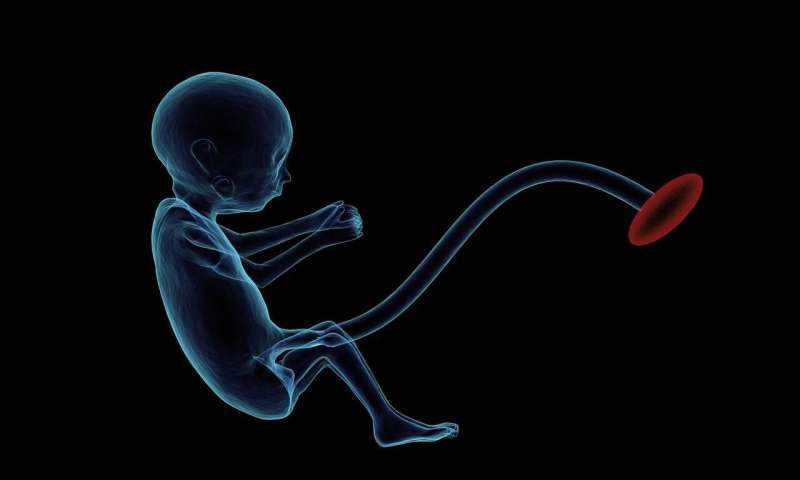
The placenta is an organ that provides the fetus with oxygen and nutrients and removes waste products. It also produces hormones, including high levels of ALLO in late pregnancy that may influence brain development. Penn, now the L. Stanley James Associate Professor of Pediatrics at Columbia University Vagelos College of Physicians and Surgeons and chief of neonatology at Columbia and NewYork-Presbyterian Morgan Stanley Children’s Hospital, coined the term “neuroplacentology” to describe this new field of research connecting placental function to brain development.
About one in 10 infants is born prematurely (and is thus deprived of normal levels of ALLO and other hormones), and many more pregnancies have poor placental function.
For this study, the researchers created a mouse model in which they were able to selectively decrease the production of ALLO during pregnancy so that some developing pups were exposed to sufficient placental ALLO while others were not. Although male and female fetuses were both subjected to ALLO deficiency, only male mice showed autism-like behaviors after birth. Working with collaborators in Washington, D.C., France, and Canada, the Penn laboratory analyzed brain development and long-term behavioral outcomes in the offspring.
ALLO reduction led to cerebellum changes, autism-like behaviors
The male mice that lacked placental ALLO had structural changes in the cerebellum, a brain region that coordinates movement and has been linked to autism, while their littermates did not.
“In particular, we observed thickening of the myelin sheaths, the lipid coating that protects nerve fibers and speeds up neural signaling,” Vacher says. The same type of thickening is also known to occur transiently in the cerebellum of some boys with autism.
The degree of myelin thickening in juvenile male mice correlated with abnormal behavior, the researchers also found. The more the sheath was thickened (as measured by myelin protein levels), the more the male mice exhibited autism-like behaviors, such as decreased sociability and repetitive activities.
“Our experimental model demonstrates that losing placental ALLO alters cerebellar development, including white matter development. Cerebellar white matter development occurs primarily after birth, so connecting a change in placental function during pregnancy with lingering impacts on later brain development is a particularly striking result,” says Penn.
“The findings provide a new way to understand poor placental function. Subtle but important changes during pregnancy or after delivery may set in motion neurodevelopmental disorders that children experience later in life.”
Similarities with human tissue
To determine if similar changes occur in infants, the researchers also examined post-mortem cerebellar tissues from preterm and full-term infants who had died soon after birth. Analysis of these human tissues showed similar changes in brain proteins when cerebellum from male babies born preterm were compared to male full-term babies.
“This study is an important first step in understanding how placental hormones may contribute to specific human neurobehavioral outcomes. We look forward to continuing our collaboration with Dr. Penn and her team to help define how cerebellar neurons and glia respond to environmental factors, including placental function, that can compromise the developing brain,” says study co-author Vittorio Gallo, Ph.D., interim chief academic officer at Children’s National Hospital and interim director of the Children’s National Research Institute.
Hormone injection reduced autism symptoms
ALLO’s therapeutic potential was then tested in the preclinical model.
Male offspring of mice given a single injection of ALLO in late pregnancy had fewer autism-like behaviors, the researchers found. Similar results were seen after an injection of muscimol, a drug that enhances the function of GABA receptors—the same receptors that respond to ALLO. Myelin protein levels in the developing cerebellum also normalized with the treatment.
“Identifying when key hormone levels are abnormal, and figuring out how and when to adjust these levels, provides an opportunity to intervene,” Penn says. “Performing additional studies with our mouse model, and measuring hormone levels in moms and babies, may lead to earlier treatment to reduce or prevent long-term cognitive and behavioral impairments in high-risk fetuses and newborns.”
Source: Read Full Article




