New Data, Film Highlight Islet Cell Transplantation Progress
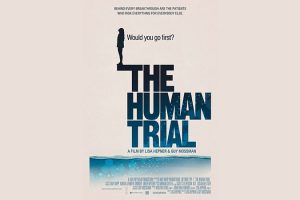
New data and a new documentary called “The Human Trial” together illuminate the hard work, sacrifice, and slow, iterative progress in the long search for a biological cure for type 1 diabetes.
Opening in select theaters on June 24, the film was written by Los Angeles filmmaker Lisa Hepner, who has type 1 diabetes, and codirected by Hepner and her husband Guy Mossman, who also filmed it. The couple co-own a film production company.
“The Human Trial” follows the personal journeys of two of the first participants in ViaCyte’s early phase 2 trial of stem-cell derived islet cell transplants, as well as those of the investigators and Hepner herself, who narrates and appears in the film, interweaving her own experience with type 1 diabetes while acting as a “bridge” between the trial’s participants and scientists. The film spans 7 years of the trial.
The timing of the film’s opening happens to follow presentations at two major medical meetings earlier this month of more recent islet cell transplantation data from ViaCyte and two other companies, Sernova and Vertex. Each is taking a different practical approach, with the most effective and safe technique yet to be determined.
But all are pursuing the same goal: a biological “cure” for type 1 diabetes with the aim of restoring fully functioning islet cells that can produce insulin and keep blood sugar levels in target range. Ultimately, the hope is to eliminate the need for both exogenous insulin and immunosuppression for all people with type 1 diabetes.
“Cell therapy is an attempt to drastically and substantially change the paradigm of how we actually treat type 1 diabetes,” Manasi S. Jaiman, MD, pediatric endocrinologist and chief medical officer at ViaCyte, said during a presentation at ENDO 2022: The Endocrine Society Annual Meeting.
Transplantation of cadaver-derived pancreatic islet cells to treat type 1 diabetes dates back more than 20 years to the landmark Edmonton Protocol, with many refinements since. About 1500 recipients have received them, and roughly a quarter has maintained insulin independence after 10 years, Jaiman said.
More recently, islets derived from stem cells — either embryonic or autologous — have been used to address the supply and quality problems that arise from cadaveric (dead) donors.
Still, though, the need for lifelong immune suppression means the only current recipients are people with type 1 diabetes for whom the risk of diabetes outweighs that of immune suppression, such as those with hypoglycemic unawareness or extreme glucose swings.
Many research efforts are underway to counter the need for immune suppression by a variety of techniques including cell encapsulation or gene modification.
While the data thus far are encouraging, most of the reports align with what Hepner says in the film: “We all want stories with a beginning, middle, and end where all the loose pieces fit together. But clinical research is messy and hard. It doesn’t fit into a tidy headline, no matter how much you want it to.”

Filmmaker Lisa Hepner, who has type 1 diabetes, checks her blood sugar.
Companies Use Different Approaches for Transplanting Islets
At ENDO 2022, Jaiman presented results for three patients who received pancreatic precursor (PEC-01) cells derived from ViaCyte’s proprietary pluripotent stem cell line. The cells are housed in an open delivery device about the size of a standard bandage to allow direct vascularization and are implanted in a patient’s forearm. An earlier version of the device was used in the two patients in “The Human Trial.”
All three patients experienced improved blood glucose levels with lower daily insulin doses and a rise from undetectable C-peptide to levels above 0.3 ng/mL. Of the three, the best results were seen in a 52-year-old woman with type 1 diabetes for 36 years complicated by hypoglycemic unawareness. At 1-year post-transplant, her A1c dropped from 7.4% to 6.9%, and time-in-range [of ideal blood glucose] from 55% to 94%, plus she had a reduction in daily exogenous insulin use of 70%. However, at 18 months her time-in-range had dropped to about 75%.
“We are watching very closely to see what this means,” Jaiman said.
Further optimization of the approach is planned. “We’re still waiting on the bulk of the data and analyzing it…We do realize this is a journey but we’re very excited by where we are,” she enthused.
In February 2022, ViaCyte announced it had teamed up with CRISPR Therapeutics to develop an allogeneic, gene-edited stem cell-derived product designed to produce insulin while at the same time evading the immune system.
Preliminary data from another company, Sernova, using a pouch device were presented at the American Diabetes Association (ADA) 82nd Scientific Sessions by Piotr j. Bachul, MD, of the Transplantation Institute at the University of Chicago, Illinois.
The Sernova Cell Pouch System containing cadaver islets was successfully transplanted into the abdominal wall of six of seven patients. After waiting a month to allow for vascularization, the cells are then placed into the pouch (as opposed to ViaCyte’s method where they are implanted together). The first three patients achieved islet cell graft function — with positive C-peptide — for up to 1 year, although all also required supplemental transplants into the portal vein to achieve insulin independence.
In May 2022, Sernova announced a partnership with Evotec to develop a product that will combine induced pluripotent stem cell (iPSC)-based beta cells for use with the Cell Pouch System.
Clinical testing is scheduled to begin in 2024, a Sernova representative told Medscape Medical News.
And as Medscape Medical News reported earlier in June, findings from Vertex Pharmaceuticals showed success in two patients who received that company’s investigational allogeneic stem-cell derived islets (VX-880), with the first person completely insulin-independent 9-months post-transplant.
In contrast to the other two companies, Vertex’s approach is to transplant the cells directly to the hepatic portal vein rather than into a subcutaneous pouch.
“The only space that has ever worked efficiently for islets is the liver because they immediately get blood…The subcutaneous space is an interesting place, but the problem is it’s not very well-vascularized,” James F. Markmann, MD, PhD, chief of the division of transplant surgery at Massachusetts General Hospital, Boston, who worked on the Vertex trials, told Medscape Medical News.
However, the Sernova representative countered: “With the Cell Pouch transplant, not only can surgeons avoid the risks associated with [hepatic] portal vein infusion — including immediate blood-mediated inflammatory reaction, which is known to kill a large proportion of infused islets — but also liver pathologies.”
Furthermore, the cells remaining in the pouch “may be entirely removed from the patient in the event of a subsequently detected cell quality issue,” which isn’t possible with cells delivered into the portal vein.
“I think it will be interesting how it plays out,” Markmann said, referring to the field as a whole.
“The Human Trial” Spotlights the Real People Behind the Data
“The Human Trial” ties together the lives of two young adult study participants: a mother named Maren Badger, who qualified for the study because she regularly experienced severe low blood sugar accompanied by seizures, and Greg Romero, a father who has sight-threatening diabetic retinopathy and other complications, as well as financial hardship.
The film chronicles their experiences over 7 years after receiving the transplant. It’s not easy for either of them to undergo all the implantation and explantation procedures as well as cope with the uncertainty as to whether the transplanted cells are working.
At the same time, the researchers’ emotional and sometimes frustrating journey is shown, as are scenes following company executives to Saudi Arabia and Japan in their pursuit of trial funding.
Hepner herself is featured pursuing the film’s storyline by frequently questioning company executives, in person and virtually, as well as telling her own story.
A visit to the Banting House Historic Site in London, Ontario, with her young son gives Hepner the opportunity to explain that after Canadian surgeon Frederick Banting discovered insulin, he sold the patent to the University of Toronto for one dollar.
“One hundred years ago, insulin wasn’t a business. It was a medical breakthrough that saved millions of lives. When Banting accepted his Nobel [Prize], he famously said, ‘Insulin doesn’t belong to me, it belongs to the world.’…Now, there’s a $245 billion industry designed to manage our disease,” Hepner says in the film.
But, she adds, “There’s a catch-22: biotech needs big pharma’s profits to fund clinical trials. Without that support the researchers wouldn’t have gotten this far. Like most relationships, it’s complicated.”
Nonetheless, the film ultimately uplifts. As one company executive says: “Data show the product is producing insulin in patients for the first time…This is a big deal. We know now that the cells work.”
“We didn’t know that 5 years ago. All the pieces are there, it’s just a matter of completing the puzzle.”
The ViaCyte work presented by Jaiman received funding from the European Commission Horizon 2020, the California Institute for Regenerative Medicine, and the JDRF. Jaiman is an employee of ViaCyte. The Sernova work was funded by Sernova and JDRF. Markmann has reported serving on advisory boards for iTolerance, eGenesis, and Qihan Biotech, and being a consultant for Vertex Pharmaceuticals. Hepner and Mossman run LA-based Vox Pop Films, a production company specializing in nonfiction content and commercials. “The Human Trial” was made in collaboration with the nonprofit Beyond Type 1.
Miriam E. Tucker is a freelance journalist based in the Washington, DC, area. She is a regular contributor to Medscape, with other work appearing in The Washington Post, NPR’s Shots blog, and Diabetes Forecast magazine. She is on Twitter: @MiriamETucker.
For more diabetes and endocrinology news, follow us on Twitter and Facebook.
Source: Read Full Article




