SARS-CoV-2 can alter bone marrow macrophage (BMM)-to-osteoclast differentiation, study finds

The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is primarily a respiratory illness.
However, as the pandemic evolves, scientists have observed a range of different ways that the virus can affect the body. Alongside the lungs, SARS-CoV-2 has been seen to affect other organs, including the heart, brain and gastrointestinal tract.
Now, a team of researchers in China and Australia has shown that SARS-CoV-2 infection can affect bone marrow macrophage (BMM)-to-osteoclast differentiation, which may impact the skeletal system.
In the current study, which appeared on the pre-print server bioRxiv*, the team found that authentic SARS-CoV-2 could efficiently infect both human and mouse BMMs and alter the expression of macrophage chemotaxis and osteoclast-related genes.
COVID-19 effects
The COVID-19 pandemic continues to spread worldwide. To date, over 138.63 million cases have been reported, and more than 2.97 million people have died.
In this infection, patients develop various clinical manifestations, including severe acute pulmonary disease, liver dysfunction, kidney injury, heart damage, pancreatic and gastrointestinal symptoms, and loss of smell or taste.
However, scientists have not yet determined the effect of COVID-19 on the skeletal system. Past evidence showed the incidence of COVID-19-associated calcium metabolic disorders and osteoporosis.
Clinicians have also observed that severely ill COVID-19 patients can have decreased blood calcium and phosphorus levels, compared with those experiencing moderate symptoms. This suggests that SARS-CoV-2 could also infect the skeletal system.
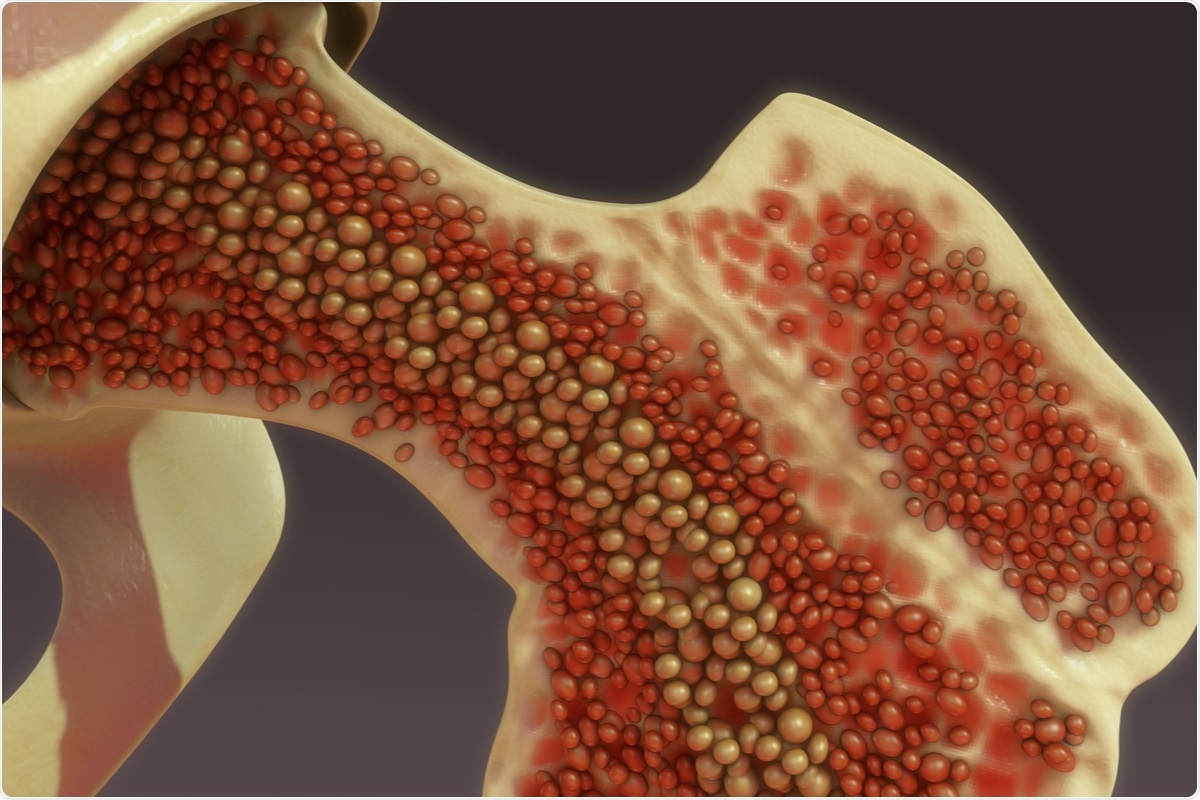
Osteoclasts are major cell types found in bones. Dysfunction in these cells may cause disturbed bone metabolism, including osteoporosis, which is characterized by decreased bone calcium and phosphorus levels.
Osteoclasts generate from the fusion of bone marrow from macrophage (BMM) precursors in the presence of macrophage colony-stimulating factor (M-CSF) and receptor activator of nuclear factor kappa-B ligand (RANKL)16.
Meanwhile, macrophages sense and respond to viral infection and maintain tissue homeostasis. When macrophage response is altered, it can lead to the rapid progression of COVID-19.
In SARS-CoV-2 patients, COVID-19 patient-derived macrophages contain SARS-CoV-2 nucleoproteins.
The study
In the study, the team investigated the interactions between SARS-CoV-2 and BMMS. They also found that SARS-CoV-2 could efficiently infect BMMs through the NRP1-dependent manner.
Further, the team characterized SARS-CoV-2 infection in BMMs and showed that NRP1 played a significant role during infection. This could pave the way to better understand the causal link between COVID-19 and bone metabolism.
The team analyzed the expression of nucleocapsid protein in control and infected BMMs to determine the infectivity of SARS-CoV-2. They also conducted SMART transcriptomic analysis, finding that authentic SARS-CoV-2 genes were markedly expressed in infected mouse BMMs, with nucleocapsid genes having the highest expression.
Interestingly, the researchers also found that the entry of SARS-CoV-2 on BMMs relied on the expression of NRP1, rather than the widely known angiotensin-converting enzyme 2 (ACE2) receptor.
Distinct from brain macrophages that exhibited aging-dependent NRP1 expression, BMMs from neonatal and aged mice had constant NRP1 expression, making them susceptible target cells for SARS-CoV-2 infection. The study suggests that NRP1 can mediate SARS-CoV-2 infection in BMMs.
The team recommends further studies and more comprehensive analysis to help clarify SARS-CoV-2’s impact on the skeletal system, which may also help discover new treatments for COVID-19, especially those experiencing long-term symptoms.
The COVID-19 pandemic remains a global health threat. Determining potential impacts on the human body can help reduce the number of deaths tied to infection.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) – https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
- Hong, G., Hong, M., Jing, S., Hao, L., Yuege, H. et al. (2021). Neuropilin-1 Mediates SARS-CoV-2 Infection in Bone Marrow-derived Macrophages. bioRxiv. doi: https://doi.org/10.1101/2021.04.14.439793, https://www.biorxiv.org/content/10.1101/2021.04.14.439793v1
Posted in: Medical Science News | Medical Research News | Miscellaneous News | Disease/Infection News | Healthcare News
Tags: ACE2, Aging, Angiotensin, Angiotensin-Converting Enzyme 2, Blood, Bone, Bone Marrow, Brain, Calcium, Cell, Coronavirus, Enzyme, Gastrointestinal Tract, Genes, Heart, Kidney, Ligand, Liver, Lungs, Macrophage, Metabolic Disorders, Metabolism, Osteoclast, Osteoporosis, Pandemic, Protein, Receptor, Respiratory, Respiratory Illness, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Virus

Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by heart. She graduated with honors (Cum Laude) for her Bachelor of Nursing degree at the University of Baguio, Philippines. She is currently completing her Master's Degree where she specialized in Maternal and Child Nursing and worked as a clinical instructor and educator in the School of Nursing at the University of Baguio.
Source: Read Full Article




