Study suggests making COVID vaccines based on Mu variant

The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Mu variant (B.1.621, B.1.621.1) has been tagged as a Variant Being Monitored (VBM), and as of August 30, 2021, it had been detected in 39 countries.
Colombia was identified as the epicenter of SARS-CoV-2 infection caused by the Mu variant. A huge surge of COVID-19 cases was reported in Columbia between March and July 2021, and SARS-CoV-2 infections caused by the gamma variant were found to be prevalent during the early stages of the surge. However, by May, the infections due to the Mu variant became dominant in Columbia.
Reports from WHO suggest that the Mu variant bears mutations that increase the risk of resistance to currently available vaccines and that further investigations are required in this area. The Mu variant is still not considered as a variant of concern by WHO.
The scientists in the present study have earlier demonstrated that the Mu variant exhibits resistance to antibodies produced in response to natural SARS-CoV-2 infection and the anti-SARS-CoV-2 vaccine Pfizer-BioNTech (BNT162b2).
The most common mutations identified in the Mu variant include the T95I and YY144-145TSN mutations in the N-terminal domain, R346K, E484K, and N501Y mutations in the receptor-binding domain, and D614G, P681H, and D950N mutations, which occur in different regions of the spike protein.
The research, released as a preprint on the bioRxiv* server, attempted to answer the cardinal question, “what are the mutations in Mu variants that confer resistance to COVID-19 convalescent sera and vaccine sera?”
YY144-145TSN or E484K mutations contribute to the SARS-CoV-2 Mu variant’s resistance to antiviral sera
Plasmids were generated by means of site-directed overlap extension PCR, and they express the SARS-CoV-2 spike protein derivatives of parental D614G (B.1) and Mu (B.1.621) variant.
Neutralization assays were performed with a series of pseudoviruses harboring these plasmids bearing the mutations. The assay was additionally performed employing pseudovirus harboring the plasmids that express spike proteins of the Alpha, Beta, Gamma, Delta, Lambda, or Mu variants.
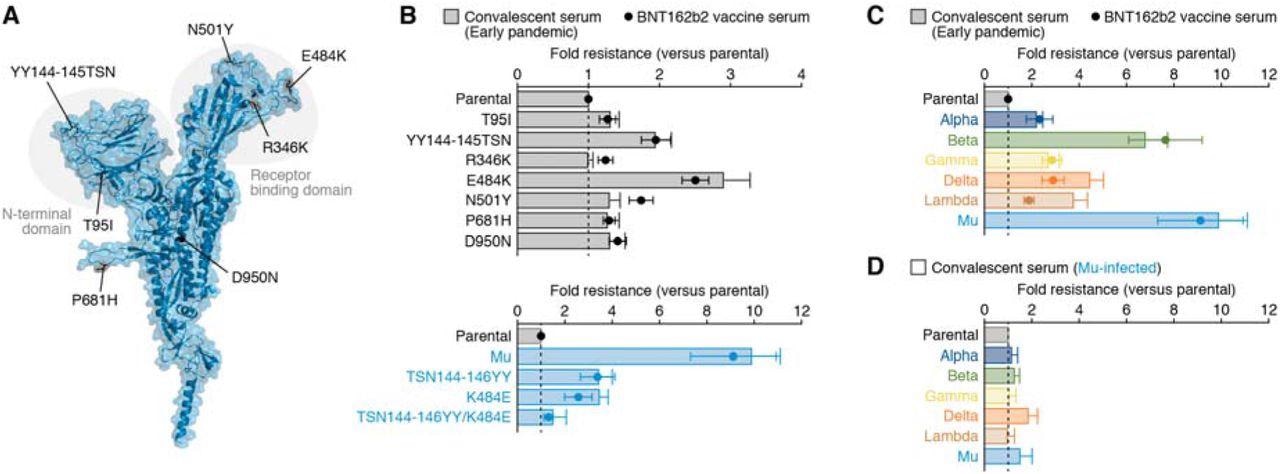
The neutralization activity of serum samples collected from 15 COVID-19 convalescent individuals who were infected in April 2020 during the early stages of the pandemic was tested in the virus neutralization assays. Additionally, serum samples from 14 subjects who were administered the BNT162b2 vaccine were also tested.
The scientists identified that two mutations YY144-145TSN and E484K, were responsible for the resistance to antibodies elicited by SARS-CoV-2 infection and the anti-SARS-CoV-2 vaccine.
This was further confirmed using ‘loss of function’ experiments on a series of Mu-based pseudoviruses that have lost the mutations of interest. Interestingly, it was found that reverting the YY144-145TSN or E484K mutations in the spike protein of the Mu variant resulted in a loss of neutralization resistance.
These findings suggest that the two mutations YY144-145TSN or E484K are responsible for the resistance exhibited by the Mu variants against the neutralizing antibodies.
Sera from SARS-CoV-2 Mu variant infected individuals exhibit broad-spectrum antiviral activity
Further assessment of the immunological spectrum of serum samples collected from COVID-19 convalescents was conducted in the study. The Mu variant was found to be nine times resistant to the sera collected from vaccinated individuals and convalescents who had natural SARS-CoV-2 infection during the early days of the pandemic.
Notably, the Mu variant did not exhibit resistance to sera collected from individuals infected by the Mu variant. Additionally, the sera from Mu variant infected individuals also showed broad-spectrum neutralization activity against different variants of concern such as alpha, beta, gamma and, lambda.
Conclusion
Emerging variants of SARS-CoV-2 are concerning. They need to be monitored carefully as they show increased transmissibility, pathogenicity, and have a high risk of resistance to the immune response compared to the original strains.
The scientists in the present study have shown that the Mu variant is resistant to neutralizing antibodies in the sera of COVID-19 convalescents and vaccinated individuals. Further, the sera from Mu-infected individuals showed broad-spectrum antiviral activity.
The sequence of the Mu variant can be utilized to develop vaccines that exhibit broad-spectrum antiviral activity against the original SARS-CoV-2 strain and its variants.
Further, research in this area is required to generate Mu variant-based novel vaccine candidates that can provide effective prophylactic therapy for COVID-19.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Neutralization of the SARS-CoV-2 Mu Variant by Convalescent and Vaccine Serum | NEJM. https://www.nejm.org/doi/full/10.1056/NEJMc2114706
- COVID Variants: What You Should Know. https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/a-new-strain-of-coronavirus-what-you-should-know
- Lauring, A. S. & Hodcroft, E. B. Genetic Variants of SARS-CoV-2—What Do They Mean? JAMA 325, 529–531 (2021), https://jamanetwork.com/journals/jama/fullarticle/2775006
- Uriu, K. et al. Characterization of the immune resistance of SARS-CoV-2 Mu variant and the immunity induced by Mu infection. 2021.11.23.469770, (2021) doi:10.1101/2021.11.23.469770,https://www.biorxiv.org/content/10.1101/2021.11.23.469770v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: Antibodies, Appendix, Assay, Coronavirus, Coronavirus Disease COVID-19, Immune Response, immunity, Mutation, Pandemic, Protein, Pseudovirus, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus

Written by
Dr. Maheswari Rajasekaran
Maheswari started her science career with an undergraduate degree in Pharmacy and later went on to complete a master’s degree in Biotechnology in India. She then pursued a Ph.D. at the University of Arkansas for Medical Sciences in the USA.
Source: Read Full Article




