COVID-19 severity is correlated with body composition

In a recent study posted to the medRxiv* preprint server, researchers assessed the effect of changes in the abdominal well-being and physique on coronavirus disease 2019 (COVID-19) severity using magnetic resonance imaging (MRI).
Previous studies have reported debilitating effects of COVID-19 on cardiac, respiratory, renal, liver, and pancreatic health. However, it is uncertain whether these effects occur primarily due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection or secondary to drugs, systemic inflammation, aging, mechanical ventilator use, or prolonged inactivity. Diagnostic imaging methods such as computed tomography (CT) ultrasound (USG) have been used to study COVID-19 features. However, organ-wise delineation of fat content and its effect on COVID-19 severity using MRI has been limited.

Study: Abdominal Imaging Associates Body Composition with COVID-19 Severity. TaMaNKunG | Shutterstock
About the study
The researchers conducted a prospective study to compare MRI images of COVID-19 patients to pre-pandemic MRI images of the United Kingdom Blood Bank (UKBB) longitudinal study performed after February 2021.
MRI scans of 1,800 individuals were obtained from UKBB and compared to post-COVID-19 MRI scans of 967 cases and 913 controls. The individuals were matched for age, sex, ethnicity, baseline scan date, and imaging centers. All the study participants resided within 60 kilometers of the imaging centers in Newcastle, Reading, and Stockport.
Along with the MRI images, demographic data including the sex, height, age, blood pressure, ethnicity, smoking status, body mass index (BMI), waist/hip ratio, Townsend deprivation index, and diagnosis rate of common diseases were obtained.
COVID-19 severity was determined using the International Classification of Diseases 10th Revision (ICD-10) diagnosis codes U071and U071.1. Hospitalized patients diagnosed with pneumonia or who were mechanically ventilated were also included under the severe COVID-19 category. Reported deaths due to COVID-19 were considered a severity outcome for pre-pandemic data. In addition to the matched cases and controls, 140 individuals were included in the study based on the severity analysis of the UKBB data.
Single slice MRI images, T1-weighted (T1W) pancreatic volume, and 3D segmentation data were obtained. The images were processed with convolutional neural networks (CNN) to generate the following image-derived phenotypes (IDPs): volumes of visceral adipose tissue (VAT), abdominal subcutaneous adipose tissue (ASAT), iliopsoas muscles, lungs, kidneys, liver, spleen, and pancreas. Proton density fat fraction (PDFF) values and the iron content of the pancreas and liver were also assessed.
A random forest classifier model was designed incorporating demographic data (age, height, sex, BMI) and IDPs of visceral fat, liver fat, and iliopsoas muscle volume to determine whether machine learning could be used to classify and predict COVID-19 severity.
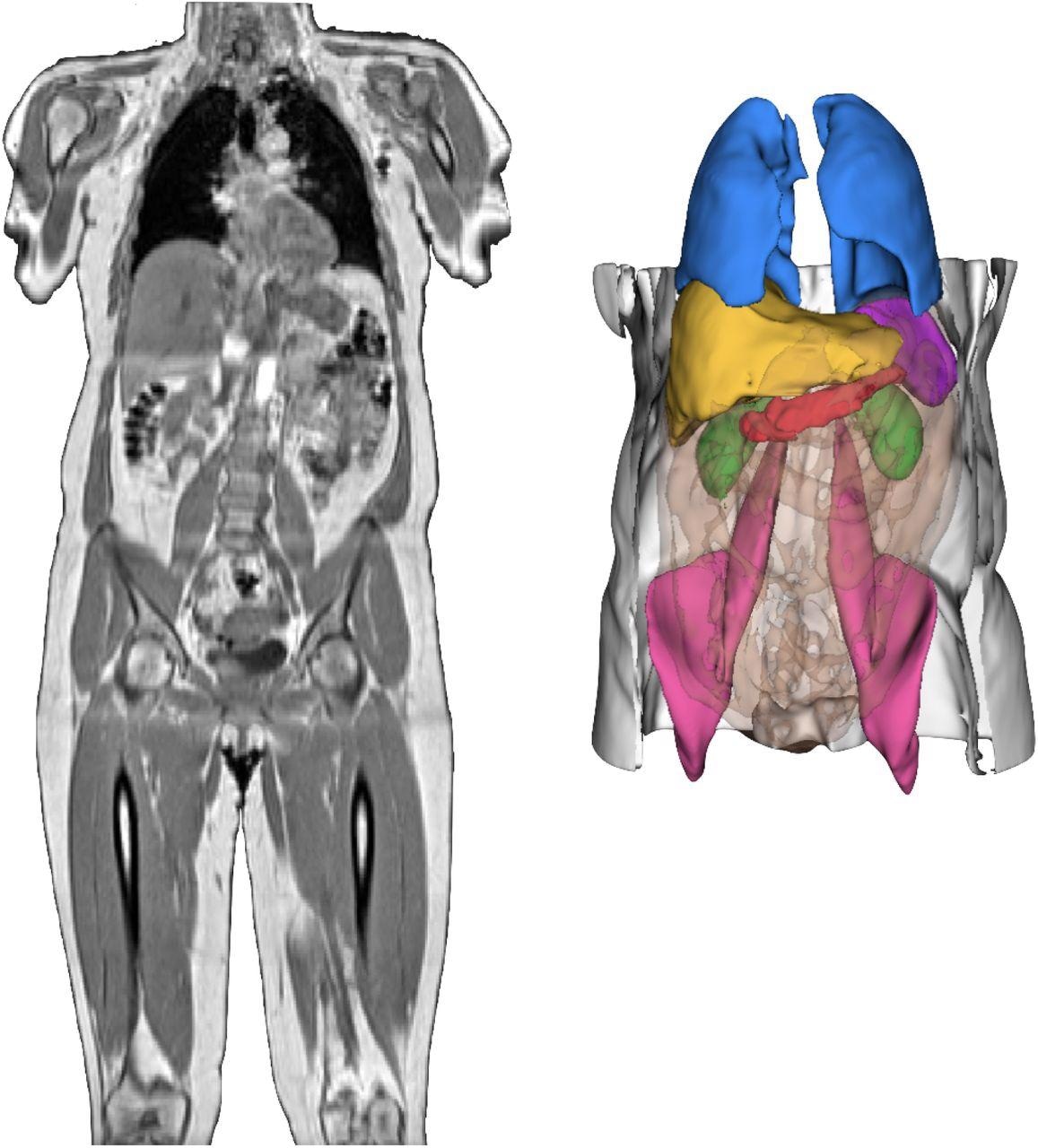
Neck-to-knee UK Biobank MRI acquisition of a COVID-19 study participant and 3D renderings of image-derived phenotypes obtained after image preprocessing and segmentation pipelines for that same participant. 3D segmentations: Liver (yellow), lungs (blue), spleen (purple), kidneys (green), abdominal subcutaneous adipose tissue (white), visceral adipose tissue (orange transparent), iliopsoas muscles (pink), pancreas (red).
Results and discussion
Only 4% of the 967 study participants had severe SARS-CoV-2 disease, of which 72% were males. Based on data analysis by the forest classifier model, the authors predicted that 5.3% of the pre-COVID imaging population would have severe COVID-19.
Increased age, BMI, waist/hip ratio, blood pressure, smoking, and the male gender were associated with the severe COVID-19. Individuals with diseases such as chronic obstructive pulmonary disease (COPD), myocardial infarction (MI), non-alcoholic fatty liver disease, and Type 2 diabetes were more prone to severe COVID-19.
A reduction in the volumes of lungs and iliopsoas muscle along with an increase in the liver and VAT volume was associated with COVID-19 severity. Elevated liver PDFF also contributed to COVID-19 disease severity. However, VAT volume most significantly contributed to COVID-19 severity.
Males may be more susceptible to severe COVID-19 than women due to higher visceral fat accumulation in men. Elevated VAT may be associated with COVID-19 severity due to increased levels of angiotensin-converting enzyme 2(ACE2) in visceral fat. Higher ACE2 levels increase the production of pro-inflammatory cytokines, contributing to the ‘cytokine-storm’ observed in COVID-19.
LAT levels may contribute to COVID-19 severity due to resultant increase in cytokine production and reduction in Vitamin D levels. In addition, LAT could also enhance viral replication due to the increased presence of ACE2 receptors. Elevated adipose content could facilitate higher intracellular utilization of lipids, increasing viral propagation.
Conclusion
The study findings demonstrated that although IDPs of liver fat, visceral fat, and muscle volume were prognostic indicators of COVID-19 severity, visceral fat was the most useful biomarker. Abdominal MRI imaging along with classifier models, could enable the identification of high-risk patients.
COVID-19 treatment strategies could be modified accordingly to provide the most appropriate therapeutic regimens to patients prone to severe disease. In addition, obese male smokers with comorbidities were most prone to severe COVID-19 based on the findings and must practice the highest level of care against COVID-19.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Abdominal Imaging Associates Body Composition with COVID-19 Severity. Nicolas Basty1 *, Elena P. Sorokin2 *, Marjola Thanaj, Ramprakash Srinivasan, Brandon Whitcher, Jimmy D. Bell1, Madeleine Cule, E. Louise Thomas. medRxiv preprint 2022, DOI: https://doi.org/10.1101/2022.02.22.22270091, https://www.medrxiv.org/content/10.1101/2022.02.22.22270091v1
Posted in: Child Health News | Men's Health News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: ACE2, Adipose, Aging, Angiotensin, Angiotensin-Converting Enzyme 2, Biomarker, Blood, Blood Pressure, Body Mass Index, Chronic, Chronic Obstructive Pulmonary Disease, Computed Tomography, Coronavirus, Coronavirus Disease COVID-19, CT, Cytokine, Cytokines, Diabetes, Diagnostic, Drugs, Enzyme, Fatty Liver, Imaging, Inflammation, International Classification of Diseases, Intracellular, Knee, Lipids, Liver, Liver Disease, Lungs, Machine Learning, Magnetic Resonance Imaging, Muscle, Myocardial Infarction, Neck, Pancreas, Pandemic, Pneumonia, Propagation, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Smoking, Spleen, Syndrome, Tomography, Type 2 Diabetes, UK Biobank, Ultrasound, Ventilator, Vitamin D

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article




