Paradigm Shift: Luspatercept for MDS
The first-in-class erythroid maturation agent luspatercept showed significant improvement over the erythropoiesis-stimulating agent epoetin alfa in reducing dependency on red blood cell transfusions among patients with lower-risk myelodysplastic syndromes (LR-MDS) who are ESA naive.
“Luspatercept is the first and only therapy to demonstrate superiority in a head-to-head study against ESAs in [transfusion-dependent] LR-MDS,” first author Guillermo Garcia-Manero, MD, chief of the MDS section, department of leukemia, at the University of Texas MD Anderson Cancer Center, Houston, said in a premeeting press briefing in advance of the annual meeting of the American Society of Clinical Oncology.
“It should be considered a paradigm shift in the treatment of LR-MDS–associated anemia,” Dr. Garcia-Manero said.
Commenting on the study, Andrew Artz, MD, a professor at the Hematologic Malignancies Research Institute, City of Hope National Medical Center, Duarte, Calif., agreed that the results could be practice changing.
“We biologically expected luspatercept to best ESA [in ring sideroblast transfusion–dependent MDS], based on luspatercept often rescuing ESA failures in this setting,” Dr. Artz said in an interview.
“The results have the potential to change initial therapy for patients with low-risk red blood cell transfusion-dependent MDS,” he said.
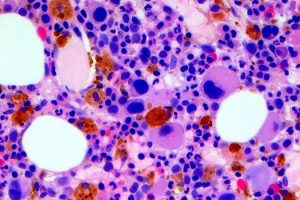
In LR-MDS, which encompasses a variety of bone marrow disorders, chronic anemia is very common, and patients, who are typically elderly, can become burdened by developing dependencies on RBC transfusions.
Transfusion dependency, in addition to creating a host of challenges, can increase the risk of death by as much as 50%, compared with patients who are not transfusion dependent, Dr. Garcia-Manero noted.
While ESAs such as epoetin alfa are the first-line treatment for LR-MDS, patients who are dependent on transfusions are less likely to respond to the agents, hence “there is an unmet need for effective and durable options other than ESAs for treating anemia in patients with LR-MDS,” Dr. Garcia-Manero said.
Luspatercept, a first-in-class monoclonal antibody, has a mechanism of action that is distinct from ESAs, modulating the transforming growth factor–beta pathway and increasing erythrocytosis.
In the previous phase 3 MEDALIST trial, the drug was shown to have efficacy over placebo in reducing the severity of anemia in LR-MDS. In 2020, in what was deemed the first advance in MDS treatment in more than a decade, those results led to approval by the Food and Drug Administration for patients with LR-MDS with ring sideroblasts who are transfusion dependent and are refractory, intolerant, or ineligible to receive ESAs.
To further investigate luspatercept’s efficacy in a head-to-head comparison with an ESA in LR-MDS patients who are ESA naive, Dr. Garcia-Manero and colleagues conducted the phase 3 COMMANDS trial.
For the global, open-label study, patients with LR-MDS who were dependent on RBC transfusions and had no prior use of ESAs were randomized 1:1 to treatment either with subcutaneous luspatercept (starting dose, 1.0 mg/kg with titration up to 1.75 mg/kg; n = 178) once every 3 weeks or subcutaneous epoetin alfa (starting dose, 450 IU/kg with titration up to 1,050 IU/kg; n = 176) once every week, for a minimum of 24 weeks.
Patients in each arm were also able to receive best supportive care, including blood transfusions. Their baseline characteristics were similar in each arm.
For the primary endpoint, patients receiving luspatercept in the intent-to-treat population were nearly twice as likely as those treated with epoetin alfa to become independent of RBC transfusions, with a concurrent mean hemoglobin increase of 1.5 g/dL or more, for at least 12 weeks in the first 24 weeks on study, at a rate of 58.5% with luspatercept versus 31.2% with epoetin alfa (P < .0001).
In addition, patients treated with luspatercept had a longer median duration of transfusion independence, at 126.6 weeks versus 77 weeks in the epoetin alfa group (hazard ratio, 0.456).
Importantly, the statistically significant improvement with luspatercept was consistent among patients with ring sideroblasts (HR, 0.626) as well as without them (HR, 0.492). Dr. Garcia-Manero noted that about 70% of patients in the study had ring sideroblasts, consistent with their common occurrence in LR-MDS.
Luspatercept was also superior in secondary endpoints, including in achieving hematologic improvement, with an erythroid response of at least 8 weeks, per International Working Group 2006 criteria, which was achieved by 74.1% with luspatercept versus 51.3% with epoetin alfa (P < .0001).
The greater improvement with luspatercept was also observed in other subgroups, including based on baseline serum erythropoietin or levels of transfusion dependence, as well as SF381 mutation status.
In terms of safety, treatment emergent adverse events (TEAEs) of any grade were reported among 92.1% of luspatercept and 85.2% of epoetin alfa patients. Longer-term posttreatment safety analyses showed no significant differences between the groups in terms of progression to high-risk MDS, in five (2.8%) with luspatercept and seven (4.0%) epoetin alfa, and progression to acute myeloid leukemia, occurring in four (2.2%) luspatercept and five (2.8%) epoetin alfa patients.
Overall rates of death between the groups were also similar during the treatment and posttreatment periods (32 [18.0%] luspatercept; 32 [18.2%] epoetin alfa patients).
“The toxicity profile was consistent with previous clinical experience,” Dr. Garcia-Manero said.
Dr. Garcia-Manero underscored that “the results of the COMMANDS trial are very important.”
“ESAs are really not optimal agents [for LR-MDS], and these results indicate that luspatercept almost doubles response rates in this patient population, therefore becoming potentially the standard of care for patients with transfusion-dependent LR-MDS who have not received prior ESA treatment,” he said.
Further commenting, Dr. Artz added that the effects in patient subgroups will be of great interest as further data on luspatercept emerges.
“Of highest interest will be the differential responses among patients with and without ring sideroblasts, as well as by SF3B1 mutational status,” he said. Furthermore, “patient-centric data emerge as even more relevant when considering the quantitatively higher rates of treatment-emergent adverse effects in the luspatercept arm.”
“We need to understand how to best sequence anemia therapies in low-risk MDS when we have two active agents, or even if [there is] a role for combined ESA/luspatercept therapy,” he noted.
“The results are exciting, but we need the final data including relevant subsets before declaring luspatercept the winner,” Dr. Artz concluded.
The study was sponsored by Celgene/Bristol-Myers Squibb. Dr. Garcia-Manero reported relationships with Abbvie, Acceleron Pharma, Aprea Therapeutics, Astex Pharmaceuticals, Bristol-Myers Squibb, Genentech, Gilead Sciences, and Novartis. Dr. Artz disclosed previous consulting relationships with Abbvie and Magenta Therapeutics.
This story originally appeared on MDedge.com, part of the Medscape Professional Network.
Source: Read Full Article




