Can ketogenic diet offer an effective alternative to antiseizure medication in infants with drug-resistant epilepsy?

In a recent study published in The Lancet Neurology, researchers evaluated the effectiveness of ketogenic diets compared to anti-seizure medications in lowering seizure frequency among newborns with drug-resistant epilepsy.
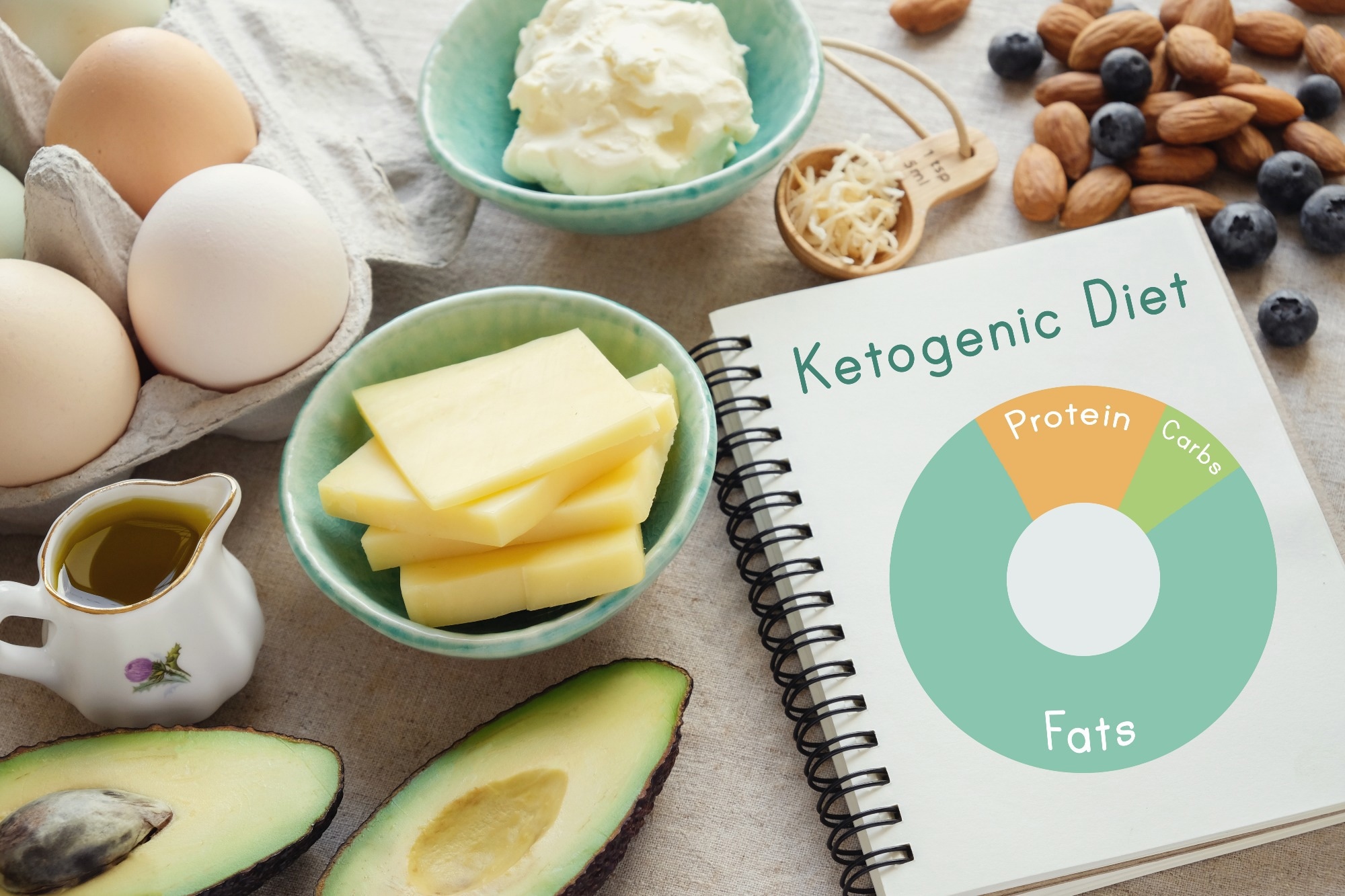 Study: Classic ketogenic diet versus further antiseizure medicine in infants with drug-resistant epilepsy (KIWE): a UK, multicentre, open-label, randomised clinical trial. Image Credit: SewCreamStudio/Shutterstock.com
Study: Classic ketogenic diet versus further antiseizure medicine in infants with drug-resistant epilepsy (KIWE): a UK, multicentre, open-label, randomised clinical trial. Image Credit: SewCreamStudio/Shutterstock.com
Background
Epilepsy is commonly observed in the first two years of life, and young children are especially vulnerable to long-term neurological damage. Although early seizure management improves developmental outcomes, many infant epilepsies have a poor prognosis.
A ketogenic diet, which is high in fat and low in carbohydrates, is a non-drug therapy option for drug-resistant epilepsy. Previous research has shown that it can increase seizure reduction and independence among pediatric and adult individuals recalcitrant to anti-seizure medications.
About the study
In the present phase 4, open-label, multicenter, open-label, randomized clinical trial, researchers assessed the effectiveness of a ketogenic diet on the number of seizures per day compared to anti-seizure medicine among infants aged below two years with drug-recalcitrant epilepsy.
The study included infants aged less than two years with drug-refractory epilepsy (described as 4.0 seizures each week unresponsive to two previous pharmacological treatments such as corticosteroids and anti-seizure medicines) from 19 United Kingdom (UK) hospitals.
The team excluded individuals with metabolic conditions that contradict ketogenic diets, progressing neurological diseases, severe gastroesophageal reflux disease, or past therapy with ketogenic diets.
After one to two weeks of observation, subjects were randomized to the ketogenic diet group or the anti-seizure drug group for eight weeks using computer-generated procedures with no stratification. Pediatric care nurses were uninformed of their group assignment, but study participants were.
The primary study outcome of the study was the seizure count each day (median) from the sixth and eighth weeks. Seizure-free infants, responder rate, food tolerability, and the link between medium-chain fatty acid content and seizure control were all secondary outcomes. After one year, the team evaluated treatment retention, life quality, and neurodevelopmental outcomes.
The team used the Vineland Adaptive Behaviour Scales (Vineland-II) and the Infant Toddler Quality of Life Questionnaire (ITQOL-97) to assess infants. The study included intention-to-treat analyses and follow-up evaluations at four weeks, eight weeks, six months, nine months, and a year.
Clinical reviews, physical examinations, documenting of seizure frequency, adverse events, medicines, laboratory investigations, tolerability questionnaire completion by parents or guardians, and completion of ITQOL-97 and Vineland-II were all part of the assessments.
The study concluded before all individuals completed the one-year follow-up due to slow enrolment and a lack of financing.
Pediatric dietitians estimated the diet components for ketogenic diet newborns, considering food diary, daily calorie needs, protein intake, and supplementation. The researchers used growth tracking, seizure diaries, and urine measures to make adjustments.
Results
Between January 2015 and September 2021, 155 newborns were screened for eligibility, and 136 were randomized to the ketogenic diet (n=78) or the anti-seizure medication group (n=58). The median follow-up duration was 11 months.
During the sixth to eighth weeks, the count of seizures each day (median) was comparable between ketogenic diet followers (five per day) and anti-seizure drug recipients [three per day; incidence rate ratio (IRR), 1.3].
At eight weeks, among 28 (44%) of the 63 ketogenic diet followers with relevant information for the intent-to-treat assessments, seizures reduced by >50% compared to 19 out of 47 (40%) anti-seizure drug recipients.
Eleven percent (seven out of 63 newborns) of ketogenic diet followers had no seizures, compared to 13% (six out of 48 infants) of anti-seizure drug recipients. At one year, no changes were observed across groups, except the child's temperament and mood and their ability to befriend others, which favored the anti-seizure drug group.
At eight weeks, ketogenic diet followers had higher ITQOL-97 ratings than the anti-seizure drug group for seven out of twelve concepts. However, general views of the child's health were quantitatively higher in the anti-seizure drug group.
At one year, parents or guardians of ketogenic diet followers evaluated their health to be considerably better than the anti-seizure drug group. The general daily life v-scale score nominally improved among anti-seizure drug recipients.
In both study groups, a comparable percentage of children encountered one or more significant adverse events [51% (40 out of 78) of ketogenic diet followers and 45% (26 of 58) anti-seizure drug recipients]. In both groups, seizures were the most prevalent major adverse events.
Three newborn fatalities occurred among ketogenic diet followers: one with dystonic-type cerebral palsy who died abruptly, one at home, and one after regular surgery under anesthesia, all of which were ruled unrelated to therapy.
Compared to the ketogenic diet group, infants in the anti-seizure medication group reported more changes in concomitant anti-seizure drugs, such as dosage increases or short courses owing to epileptic escalation or prophylaxis for planned hospitalization.
Conclusion
Overall, the study findings showed that, although equivalent in tolerance and efficacy to anti-seizure drugs, the ketogenic diet proved safe and successful in treating newborns with drug-recalcitrant epilepsy, enhancing the quality of life and neurodevelopment.
However, more cohort studies and different study designs are required to assess the advantages and risks of the diet.
-
Natasha E Schoeler et al., (2023) Classic ketogenic diet versus further anti-seizure medicine in infants with drug-resistant epilepsy (KIWE): a UK, multicentre, open-label, randomised clinical trial, Lancet Neurol, doi: https://doi.org/10.1016/S1474-4422(23)00370-8. https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(23)00370-8/fulltext
Posted in: Child Health News | Medical Science News | Medical Research News | Medical Condition News
Tags: Cerebral Palsy, Children, Clinical Trial, Diet, Drugs, Efficacy, Epilepsy, Food, Frequency, Gastroesophageal Reflux Disease, Ketogenic Diet, Laboratory, Medicine, Neurology, Newborn, Prophylaxis, Protein, Research, Seizure, Surgery

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.




