New tool to predict peoples risk of developing lung cancer within the next ten years

Researchers at the University of Nottingham have helped to develop a new tool called “CanPredict,” which is able to identify the people most at risk of developing lung cancer over the next 10 years, and put them forward for screening tests earlier, saving time, money and, most importantly, lives.
Featured in the journal Lancet Respiratory Medicine, the researchers worked with colleagues at the University of Oxford to develop and test the tool using the anonymized health records of more than 19 million adults from across the U.K.
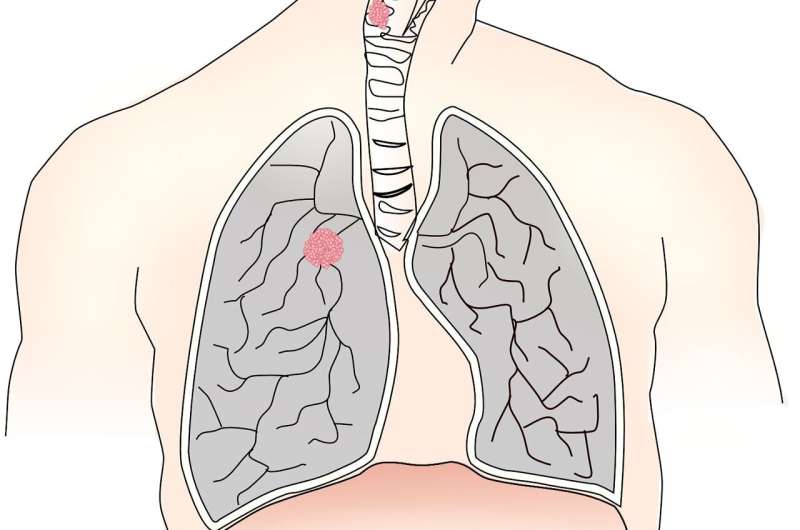
Lung cancer is the second most common cancer in incidence and the leading cause of cancer deaths worldwide. However, lung cancer screening—”catching it early”—has been shown to improve survival rates. Because of this, in September 2022 the U.K. National Screening Committee recommended using targeted lung cancer screening. However, the committee did not recommend which tools would best be used for targeting screening at people most at risk.
“We set out to develop a tool that could be used to identify people at highest risk of developing lung cancer based on data already recorded in their medical records. The tool performed well when we tested it in a separate group of people, and appeared to be better at identifying people who would go on to develop lung cancer than some other approaches. It could help to inform prioritization of people for targeted lung cancer screening in the U.K. and so enable diagnoses to be made at an earlier stage,” says Carol Coupland, one of the study co-authors.
Current methods to target screening rely on doctors recognizing high-risk individuals or using tools based on using patient questionnaires to score risk and put those at highest forward.
David Baldwin, Honorary Professor of Medicine and Consultant Physician in the School of Medicine added, “In targeted lung cancer screening the object is only to screen those who are more likely to develop the condition. This avoids harm in people at low risk and increases cost effectiveness. Much research has been focussed on multivariable models to predict risk of lung cancer and this model outperforms others when applied to primary care data.”
To develop the new tool the researchers used two separate sets of health record data. Using the QResearch Database—which, in total, contains the anonymized health records of more than 35 million patients, spanning all ethnicities and social groups across the U.K.—to identify 13 million people aged 25 to 84 years old, among whom 73,380 had a diagnosis of lung cancer. They then looked back through their health records to identify common factors which might be used to statistically predict their risk of developing the cancer. Factors such as smoking, age, ethnicity, body mass index, medical conditions and social deprivation (and others) were considered as part of the analysis.
Once the tool was developed, the researchers needed to test it. They did this using a separate set of anonymized GP health records—the Clinical Practice Research Datalink (CPRD).
The researchers used the CPRD data (which contained data from an additional 2.54 million people’s anonymized health records) to see which people their new tool predicted were at the greatest risk of developing lung cancer, and then compared this to those who did go on to develop lung cancer.
The new CanPredict tool correctly identified more people who went on to develop lung cancer and was more sensitive than current recommended methods of predicting risk, across 5-, 6-, and 10-year forecasts.
“Improving early diagnosis of lung cancer is incredibly important both for the NHS but especially for patients and their families. We hope that this new validated risk tool will help better prioritize patients for screening and ultimately help spot lung cancer earlier when treatments are more likely to help. We’d like to thank the many thousands of GPs who have shared anonymized data for research without whom this would not have been possible,” says Professor Julia Hippisley-Cox, senior author.
The researchers plan to make the tool publicly available for use, subject to further funding for implementation in day-to-day practice and to ensure Medicines and Healthcare Products Regulatory Agency (MHRA) medical device compliance.
More information:
Weiqi Liao et al, Predicting the future risk of lung cancer: development, and internal and external validation of the CanPredict (lung) model in 19·67 million people and evaluation of model performance against seven other risk prediction models, The Lancet Respiratory Medicine (2023). DOI: 10.1016/S2213-2600(23)00050-4
Journal information:
Lancet Respiratory Medicine
Source: Read Full Article




