Research says benefits of continuing immunization of front-line workers in BC with AstraZeneca vaccine far outweigh risks

Amidst the continued surge of coronavirus disease (COVID-19) cases, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), vaccination efforts continue to mitigate the spread of the virus.
Vaccination rollouts have commenced in many countries. One of the vaccines approved via an emergency use authorization (EUA) by the Food and Drug Administration (FDA) was the University of Oxford's AstraZeneca COVID-19 ChAdOx1 nCoV-19 SARS-CoV-2 viral vector vaccine.
As countries started using the vaccines, reports surfaced of rare instances of blood clots, with low platelets detected in some individuals inoculated with the vaccine.
A recent study by researchers at the University of British Columbia (B.C.) shows that the benefits of continuing the COVID-19 vaccine of front-line workers with the AstraZeneca vaccine outweigh the increased risk of prothrombotic thrombocytopenia.
In the study, posted to the pre-print server medRxiv*, the researchers aimed to determine the risks and benefits of delaying vaccination of front-line workers in B.C.
Increased risk of blood clots
On March 29, 2021, Canada's National Advisory Committee on Immunization (NACI) recommended against using the AstraZeneca COVID-19 vaccine in younger adults to allow for investigation of the risk for vaccine-induced prothrombic immune thrombocytopenia (VIPIT).
British Columba stopped its front-line workers' vaccination program, which used the AstraZeneca vaccine. However, the province received additional 246,700 doses of the vaccine through the U.S. and COVAX up until April 11, which are enough to provide the first dose of vaccine to all unvaccinated front-line workers.
Meanwhile, it is unclear if an alternative vaccine will be provided immediately for front-line workers, particularly healthcare personnel.
The study
To arrive at the study findings, the researchers reviewed the latest evidence to compare the expected number of deaths due to COVID-19 and VIPIT under the situations of immediately continuing vaccination of front-line workers with the AstraZeneca vaccine or delaying it in favor of mRNA vaccines.
The team also compared the individual mortality risk of receiving the AstraZeneca vaccine with delaying getting the vaccine in favor of waiting to receive an mRNA vaccine.
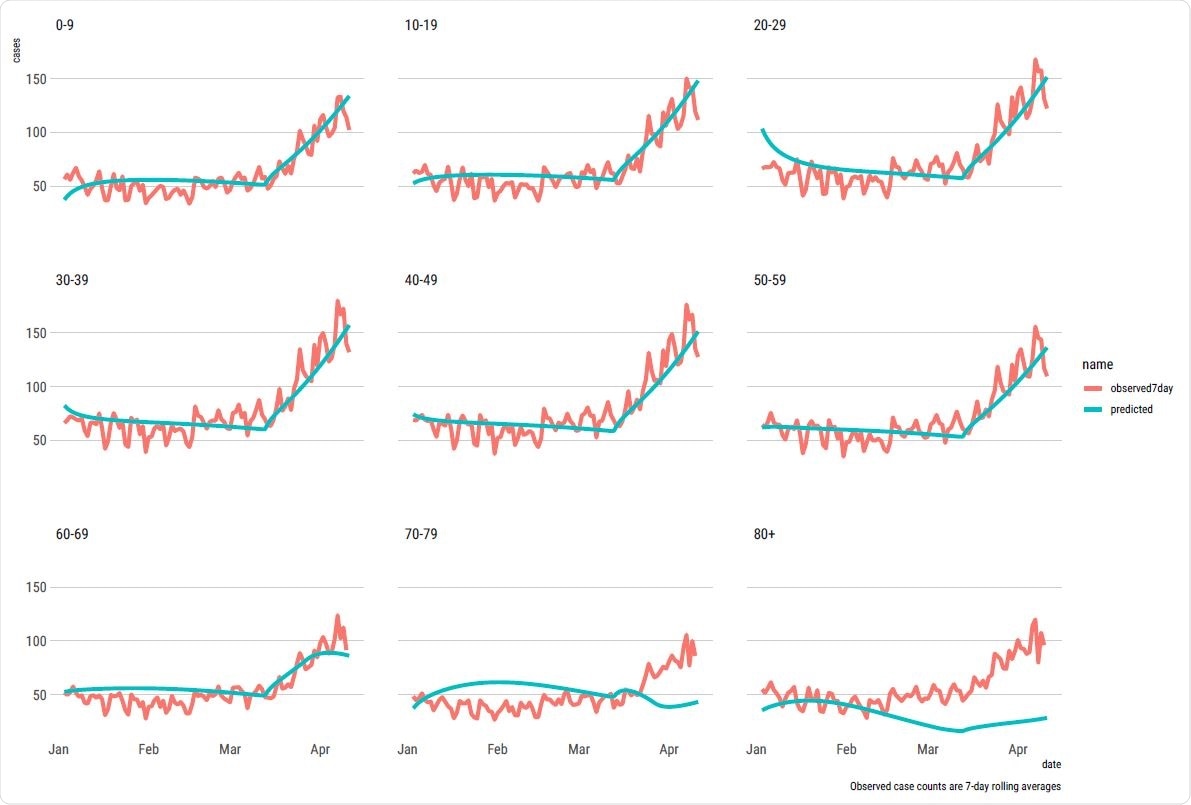
The study findings estimated that if B.C. continues with the vaccination of front-line workers with the AstraZeneca vaccine, it is expected to see about 27,000 fewer cases of COVID-19, 500 fewer hospital admissions, 80 fewer COVID-19 deaths, and 1,400 fewer cases of long COVID between April 1 and October 1, 2021, for expected VIPIT-related death of 0.674.
Further, the team found that in the same period in high transmission areas, the estimated excess risk of mortality or death due to COVID-19 and VIPIT was markedly higher in the delayed vaccination with mRNA vaccine situation than that of immediately vaccinating with the AstraZeneca vaccine for people aged 30 to 69.
For individuals below 30, however, the immediate vaccination with the AstraZeneca vaccine posed a higher risk than delayed vaccination with an mRNA vaccine.
The team noted that the analysis from an individual risk perspective reveals that the risk of getting COVID-19 and dying from it due to delayed vaccination is higher than the risk of dying from VIPIT in those over 40, and also in those over 30 years old in high-risk areas.
The study findings were based on currently available rates of 1 in a million to 1 in 100,000 for VIPIT, which might need correction if more cases of the complication are reported.
In a nutshell, the researchers concluded that the benefits of immediately vaccinating front-line workers with the AstraZeneca vaccine far outweigh the risk for people aged 40 and above and those who are 30 years old above, living in high-risk regions.
"Ultimately, in dynamic situations like this where the evidence is uncertain and evolving, vaccine rollout decisions are judgment calls that need to take a complex network of medical, epidemiological, ethical, logistics, and societal considerations into account," the researchers noted in the study.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
-
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) – https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf
- Adibi, A., Mozafarihashjin, M., and Sadatsafavi, M. (2021). Continuing COVID-19 Vaccination of Front-Line Workers in British Columbia with the AstraZeneca Vaccine: Benefits in the Face of Increased Risk for Prothrombotic Thrombocytopenia. medRxiv. https://www.medrxiv.org/content/10.1101/2021.04.11.21255138v2
Posted in: Medical Research News | Medical Condition News | Disease/Infection News | Healthcare News
Tags: Blood, Coronavirus, Coronavirus Disease COVID-19, Healthcare, Hospital, Immune Thrombocytopenia, Immunization, Mortality, Platelets, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Thrombocytopenia, Vaccine, Viral Vector, Virus

Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by heart. She graduated with honors (Cum Laude) for her Bachelor of Nursing degree at the University of Baguio, Philippines. She is currently completing her Master's Degree where she specialized in Maternal and Child Nursing and worked as a clinical instructor and educator in the School of Nursing at the University of Baguio.
Source: Read Full Article




