Study shows paxlovid can safely be used to reduce risk of severe COVID in people who are pregnant

Findings from a Johns Hopkins Medicine research study published today in JAMA Network Open provide strong evidence that people who are pregnant and have been infected with SARS-CoV-2 (the virus that causes COVID-19) can safely take the antiviral drug Paxlovid to reduce the possibility of severe disease.
“Based on our results, we feel that the benefit to both the mother and the developing fetus of preventing severe COVID outweighs any potential risks from Paxlovid therapy,” says study lead author William Garneau, M.D., M.P.H., assistant professor of medicine at the Johns Hopkins University School of Medicine.
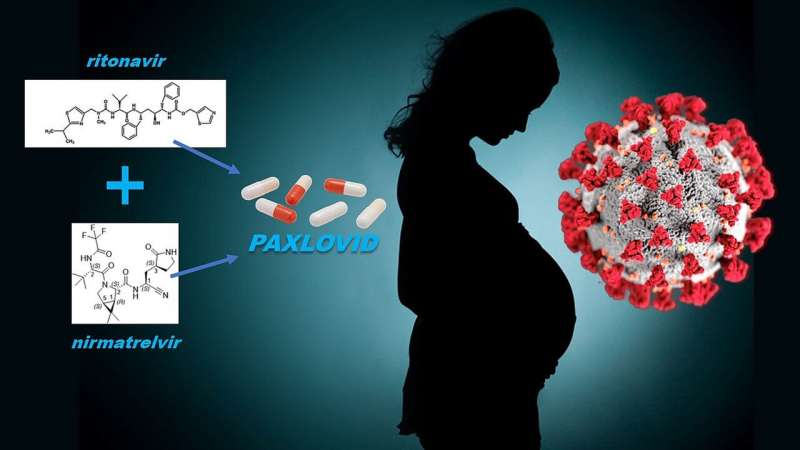
Paxlovid is an investigational agent (still under study) being used as a treatment for patients with mild-to-moderate COVID-19. It consists of two medicines: nirmatrelvir, an antiviral agent that inhibits a key enzyme that SARS-CoV-2 needs to reproduce infectious progeny, and ritronavir, a drug that enhances the action of nirmatrelvir by keeping it longer in the body.
In December 2021, the U.S. Food and Drug Administration authorized the emergency use of Paxlovid for adults and children age 12 years and older infected with SARS-CoV-2 and at high risk for progression to severe COVID, including hospitalization and death.
“The clinical trials that enabled Paxlovid to receive its emergency use authorization showed that participants were 89% less likely to develop severe illness and death; however, people who were pregnant weren’t among the participants, and pregnancy is now known to be a condition placing patients at risk of severe disease,” says co-study senior author Irina Burd, M.D., Ph.D., formerly professor of gynecology and obstetrics at the Johns Hopkins University School of Medicine and now chair of the Department of Obstetrics, Gynecology, and Reproductive Sciences at the University of Maryland School of Medicine.
In their study, the researchers selected participants from 3,442 people who were pregnant, diagnosed with mild-to-moderate COVID-19 and seen at centers within the Johns Hopkins Health Systems between March 15, 2020, and Aug. 20, 2022.
From this population, 47 people who met the study criteria were prescribed Paxlovid and monitored for outcomes and any complications. The median age of this group was 34, 17% were Black, 11% were Hispanic and the median gestational age (stage of pregnancy) was 28 weeks. The majority of participants had received at least their initial COVID vaccinations and started Paxlovid therapy within one day of symptom onset.
Ninety-six percent (45 out of 47) of the participants completed the course of therapy, tolerating it well. Of these, 25 delivered babies following the treatment. Twelve of the deliveries were done by cesarean section, and of those, nine were scheduled and not related to treatment. Two participants were hospitalized for pre-existing conditions and not severe COVID.
Overall, the incidence of maternal and fetal complications from Paxlovid were within expected limits.
“There are some limitations to our research, including the use of data from a single health system and the small population with mild COVID studied,” says Garneau. “But we believe that our study is the largest to date looking at Paxlovid’s safety and efficacy in people who were pregnant at the time of therapy, and therefore, indicates that the treatment should be an option for these patients.”
A number of medical organizations agree, including the Society for Maternal-Fetal Medicine, which states it “supports the use of Paxlovid for treatment of pregnant patients with COVID-19 who meet clinical qualifications,” and the American College of Obstetricians and Gynecologists, which lists pregnancy “among the conditions that put individuals at high risk for clinical progression [to severe COVID]. This makes pregnant patients, including those with pregnancy as their only risk factor, eligible to receive outpatient oral SARS-CoV-2 protease inhibitor therapy [Paxlovid].”
“While more study of Paxlovid is needed to confirm our findings of its safety and efficacy during pregnancy, we feel that even at this time, the medication should be strongly considered for pregnant patients who are unvaccinated or at risk for progression to severe COVID disease or not likely to have drug-drug interactions,” says co-study senior author Kelly Gebo, M.D., M.P.H., professor of medicine at the Johns Hopkins University School of Medicine.
More information:
William M. Garneau et al, Analysis of Clinical Outcomes of Pregnant Patients Treated With Nirmatrelvir and Ritonavir for Acute SARS-CoV-2 Infection, JAMA Network Open (2022). DOI: 10.1001/jamanetworkopen.2022.44141
Journal information:
JAMA Network Open
Source: Read Full Article




