Master regulator of liver metabolism identified during infection


Researchers at the CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences identified a key mechanism for how antiviral immune responses reprogram liver metabolism. Their recent study, which was published in the renowned scientific journal Immunity, investigated the communication between inflammation and liver metabolism during chronic viral infection.
Surprisingly, the antiviral cytokine type I interferon (IFN-I) was found to be a master regulator of metabolic pathways in liver cells. The researchers focused on the urea cycle, a central metabolic node, and found that it is disrupted by IFN-I during viral infection. This led to altered serum metabolite concentrations which regulated antiviral immunity and reduced liver pathology.
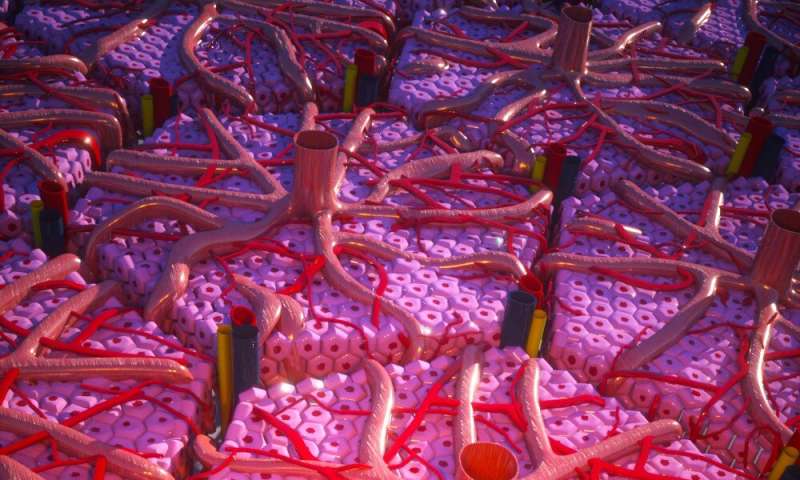
The liver is a crucial organ for systemic metabolism in our body. Apart from the turnover of biomolecules and drug metabolism, the liver’s main function is the removal of toxic substances from the organism. Hepatocytes, or liver cells, are the most abundant cell type and functional unit of the liver. They are metabolic powerhouses in the healthy organism, but they also serve as important immune signaling platforms during infections. As such, they have the potential to react to a range of cytokines—small molecules that are essential for the coordination of immune responses.
Previous studies in the field of immunology and metabolism, or immunometabolism, unveiled groundbreaking mechanisms about how cells of the immune system need to adjust their metabolism to perform their functions to fight pathogens and cancer. Building on this, Andreas Bergthaler and his group at CeMM aimed to study the immunometabolic changes that occur in the whole organism during infection. They particularly focused on the liver due to its important role in controlling systemic metabolism.

To dissect the involved complex processes, the authors took advantage of the benchmark model of chronic infection, the lymphocytic choriomeningitis virus (LCMV). Research with LCMV had already led to fundamental insights into immunology over the past 80 years, and notably contributed to three Nobel Prizes. Among them is the 2018 Nobel Prize in Physiology or Medicine, which was awarded to James Allison and Tasuku Honjo for their discoveries relating to the revolutionary new cancer immunotherapies which exploit the body’s own immune killer cells, or CD8 T cells.
The present study by Alexander Lercher, Anannya Bhattacharya et al. is the result of cross-disciplinary collaborations with researchers from the Medical University of Vienna and the University of Veterinary Medicine in Vienna (Austria), as well as from the Hannover Medical School (Germany), the Cantonal Hospital St. Gallen (Switzerland) and the company Bio-Cancer Treatment International Ltd (China). The study was designed as an integrative unbiased approach to investigate the molecular changes in the liver during chronic infection. Next to expected inflammatory changes, the authors identified intriguing changes in hepatocyte metabolism. Many central metabolic pathways, among them the urea cycle, were found to be repressed upon infection. The urea cycle is essential to remove toxic ammonia from the body to prevent brain damage.
Surprisingly, the researchers identified the antiviral cytokine signaling pathway of type I interferons (IFN-I) as a regulator of the urea cycle. This resulted in altered blood concentrations of the amino acids arginine and ornithine. “A key experiment for us was that when we removed the receptor for IFN-I on the surface of hepatocytes, we didn’t see these metabolic changes anymore,” says Alexander Lercher, first author of the study and Ph.D. student in the laboratory of CeMM Principal Investigator Andreas Bergthaler. The systemic changes of arginine and ornithine were found to inhibit antiviral CD8 T cell responses and to reduce liver damage.
One of the most important revelations of this study was the identification of IFN-I signaling as a master regulator for the repression of metabolic processes in hepatocytes upon infection. “We were really surprised that an antiviral molecule affects such vital biological processes as the urea cycle during infection,” says Michael Trauner, co-author of the study and head of the Department of Gastroenterology and Hepatology at the Medical University of Vienna. Together, these findings shed new light on how the body’s immune system evolved to regulate liver metabolism that modulate CD8 T cell responses and reduce collateral tissue damage during infection.
Source: Read Full Article




