Healthy Gut Tied to Better Cognition
A healthy, diverse gut microbiome is associated with better cognitive function in middle age, new research suggests.
Investigators conducted cognitive testing and analyzed stool samples in close to 600 adults and found that -diversity, which is a between-person measure of gut microbial community composition, was significantly associated with cognitive scores.
Three specific bacterial genera showed a positive association with performance on at least one cognitive test, while one showed a negative association.
“Data from our study support an association between the gut microbial community and measure of cognitive function — results that are consistent with findings from other human and animal research,” study investigator Katie Meyer, ScD, assistant professor, Department of Nutrition, UNC Gillings School of Public Health, Chapel Hill, North Carolina, told Medscape Medical News.
“However, it is also important to recognize that we are still learning about how to characterize the role of this dynamic ecological community and delineate mechanistic pathways,” she said.
The study was published online February 9 in JAMA Network Open.
“Novel” Research
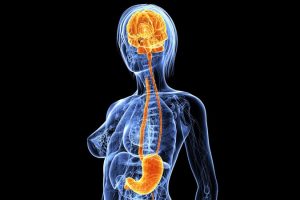
“Communication pathways between gut bacteria and neurologic function (referred to as the ‘gut-brain axis’) have emerged as a novel area of research into potential mechanisms regulating brain health through immunologic, metabolic, and endocrine pathways,” the authors write.
A number of studies have “shown associations between gut microbial measures and neurological outcomes, including cognitive function and dementia,” but mechanisms underlying these associations “have not been fully established.”
Animal and small-scale human studies have suggested that reduced microbial diversity is associated with poorer cognition, but studies have not been conducted in community-based large and diverse populations.
The researchers therefore examined cross-sectional associations of gut microbial diversity and taxonomic composition with cognitive status in a large group of community-dwelling, sociodemographically diverse Black and White adults living in four metropolitan areas who were participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study.
They hypothesized that microbial diversity would be positively associated with global as well as domain-specific cognitive status and that higher cognitive status would be associated with specific taxonomic groups involved in short-chain fatty acid production.
The CARDIA’s year 30 follow-up examination took place in 2015 – 2016, when the original participants ranged in age from 48 to 60 years. During that examination, participants took a battery of cognitive assessments, and 615 also provided a stool sample for a microbiome substudy; of these, 597 (mean [SD] age, 55.2 [3.5] years, 44.7% Black, 45.2% White) had both stool DNA available for sequencing and a complete complement of cognitive tests and were included in the current study.
The cognitive tests included the Digit Symbol Substitution Test (DSST); Rey-Auditory Verbal Learning Test (RAVLT); the timed Stroop test; letter fluency and category fluency; and the Montreal Cognitive Assessment (MoCA).
Covariates that might confound associations between microbial and cognitive measures, including body mass index, diabetes, age, sex, race, field center, education, physical activity, current smoking, diet quality, number of medications, and hypertension, were included in the analyses.
The investigators conducted three standard microbial analyses: within-person -diversity; between-person -diversity; and individual taxa.
Potential Pathways
The strongest associations in the variance tests for β-diversity, which were significant for all cognition measures in multivariable-adjusted principal coordinates analysis (all Ps = .001 except for the Stroop, which was .007). However, the association with letter fluency was not deemed significant (P = .07).
After fully adjusting for sociodemographic variables, health behaviors, and clinical covariates, the researchers found that three genera were positively associated, while one was negatively associated with cognitive measures.
| Microbiota | Association | Cognitive test | β (95% CI) |
|---|---|---|---|
| Barnesiella | Positive |
|
|
| Lachnospiraceae FCS020 group | Positive |
|
|
| Akkermansia | Positive |
|
|
| Sutterella | Negative |
|
|
“The strongest results from our study were from a multivariate analysis that can be considered a test of the overall community,” said Meyer.
She pointed to several pathways through which gut microbiota can contribute to brain health.
“We know form mechanistic studies in animal models that the gut microbiota is involved in systemic inflammation, which is a risk factor for brain pathology,” she said.
Moreover, “the gut microbiota is involved in the production of metabolites that may impact the brain, including tryptophan metabolites and short-chain fatty acids, many of which derive from dietary components, which may help explain associations between diet and cognition (eg, the Mediterranean-style diet can be protective),” she added.
Starting Point
Commenting for Medscape Medical News, Timothy Dinan, MD, PhD, professor of psychiatry and an investigator, APC Microbiome Institute, University College Cork, Ireland, said, “This is an important study, adding to the growing body of evidence that gut microbes influence brain function.”
Dinan, who was not involved with the study, continued: “In an impressively large sample, an association between cognition and gut microbiota architecture was demonstrated.”
He cautioned that the study “is limited by the fact that it is cross-sectional, and the relationships are correlational.” Nevertheless, “despite these obvious caveats, the paper undoubtedly advances the field.”
Meyer agreed, noting that there is “a paucity of biomarkers that can be used to predict cognitive decline and dementia,” but because their study was cross-sectional, “we cannot assess temporality (ie, whether gut microbiota predicts cognitive decline); but, as a start, we can assess associations.”
She added that “at this point, we know far more about modifiable risk factors that have been shown to be positively associated with cognitive function,” including eating a Mediterranean diet and engaging in physical activity.
“It is possible that protective effects of diet and activity may, in part, operate thorough the gut microbiota,” Meyer suggested.
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by the National Heart, Lung, and Blood Institute, the Intramural Research Program of the National Institute on Aging, and the University of North Carolina Nutrition Research Institute. Meyer and co-authors and Dinan report no relevant financial relationships.
JAMA Netw Open. Published online February 8, 2022. Full text
For more Medscape Psychiatry news, join us on Facebook and Twitter.
Source: Read Full Article




